Understanding male reproductive anatomy is essential – not just for performing vasectomies, but also for explaining the procedure clearly and answering questions from patients
In this discussion, we’ll start with a quick overview of the male reproductive system, then zoom in on the genital anatomy, and finally focus on the scrotal anatomy – especially the vas deferens, our main star.
We’ll keep shifting our perspective: sometimes looking at the big picture, sometimes zooming in on key details, always tying it back to how it all relates to vasectomy. Along the way, we’ll use text, photos, and diagrams to explain things from different angles, so everything makes sense on multiple levels.
The Male Reproductive System as it pertains to Vasectomy
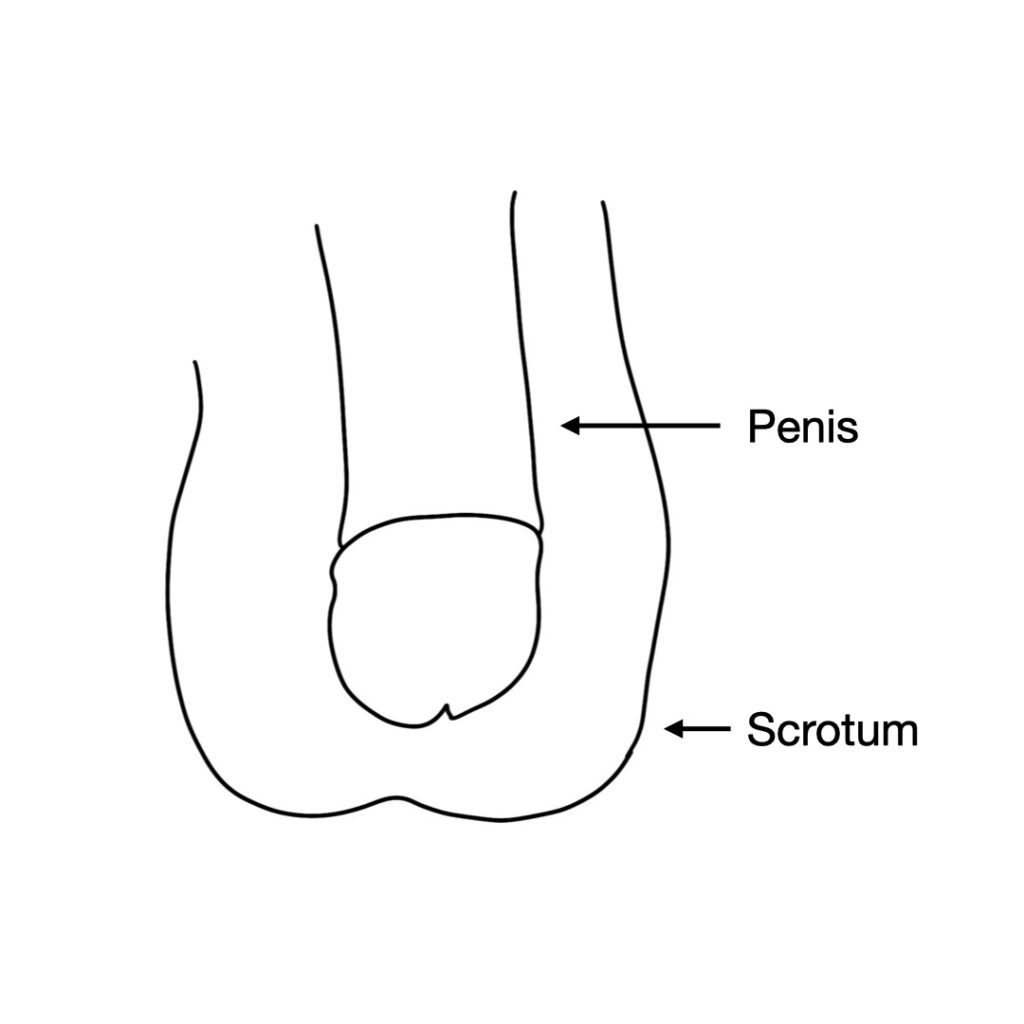
The male reproductive system is sometimes described as only the penis, scrotum, and associated organs.
A more complete discussion though, includes the brain, the nerves of the spinal cord and periphery, and the circulatory system. A familiarity of the complex interplay among these various components of the male reproductive system is vital for understanding how vasectomy works, and what does and does not change after a vasectomy.
To illustrate the big picture, we’ll look at a the famous diagram by the Italian artist Leonardo da Vinci, highlighting the various components that interact within the reproductive system.
The key point is that the reproductive system is much more than just the genitals. It’s a whole system that works together. For example, sex drive is mostly a function of the brain. Strong erections and sexual endurance are mostly a function of the circulatory system as it delivers blood to the penis. Strong muscles are mostly a function of exercise, good diet, and the influence of testosterone. As we learn more about how little a vasectomy affects each of these systems, we’ll be able to better understand the procedure.
Male Genital Anatomy
As we explore the male genitals, we’ll start by identifying the components of the genitourinary system. The diagram below labels each part and illustrates their positions relative to one another.
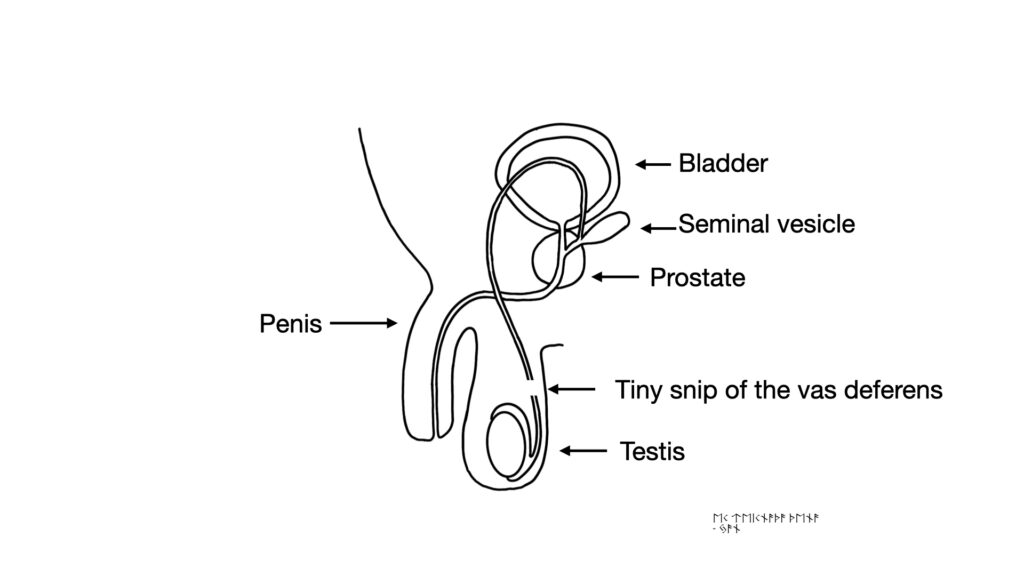
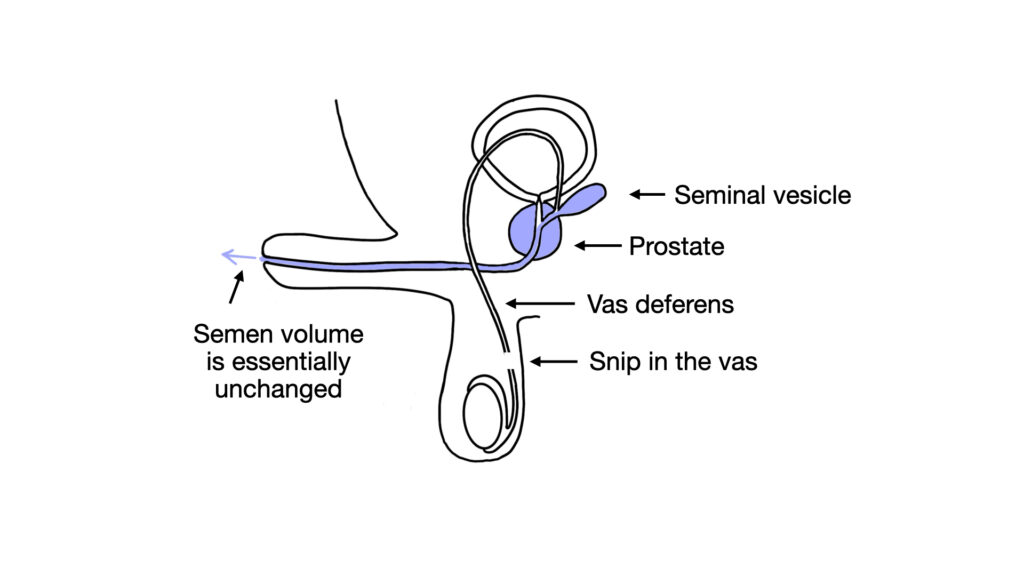
A vasectomy is a simple operation that snips and blocks the vasa deferentia, the tubes that carry sperm. Vasa deferentia is the plural of vas deferens. As we see in the diagram below, the rest of the male genitalia remains unaffected. The testes, prostate, penis, and other structures continue to function normally. Even when we take a broader view of the reproductive system to include the brain, heart, and major blood vessels, snipping the tiny vasa does not alter any of these components.
Scrotal Anatomy
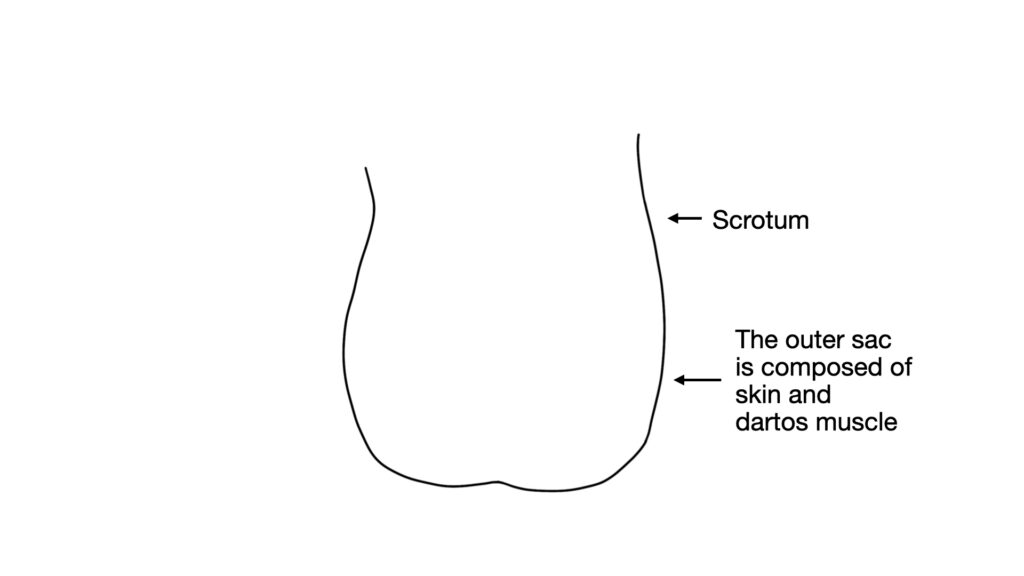
The scrotum is the sac of skin and tissue that hangs down at the base of the penis. The wall of the scrotum is composed of skin and a layer of thin muscle called the dartos muscle. This muscle can contract to raise and lower the testes. When the dartos is contracted, the skin wrinkles and the testes are raised.

Scrotum (relaxed)

Scrotum (contracted)
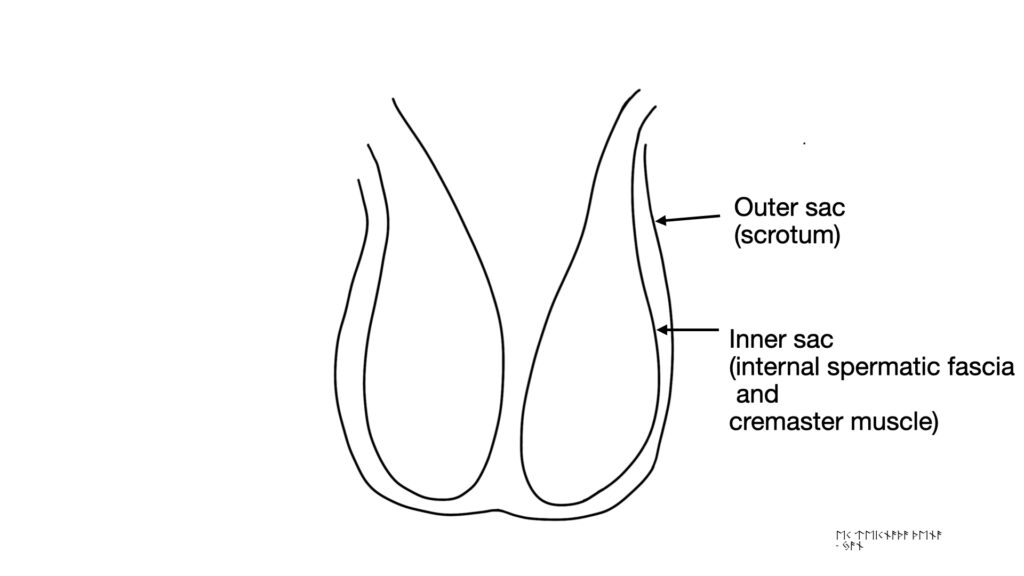
One way to conceptualize the scrotal contents is to view the outer scrotum as one large sac. This outer sac is composed of skin and dartos muscle.
In many diagrams, the testes are drawn as though they hang loosely within the scrotum.
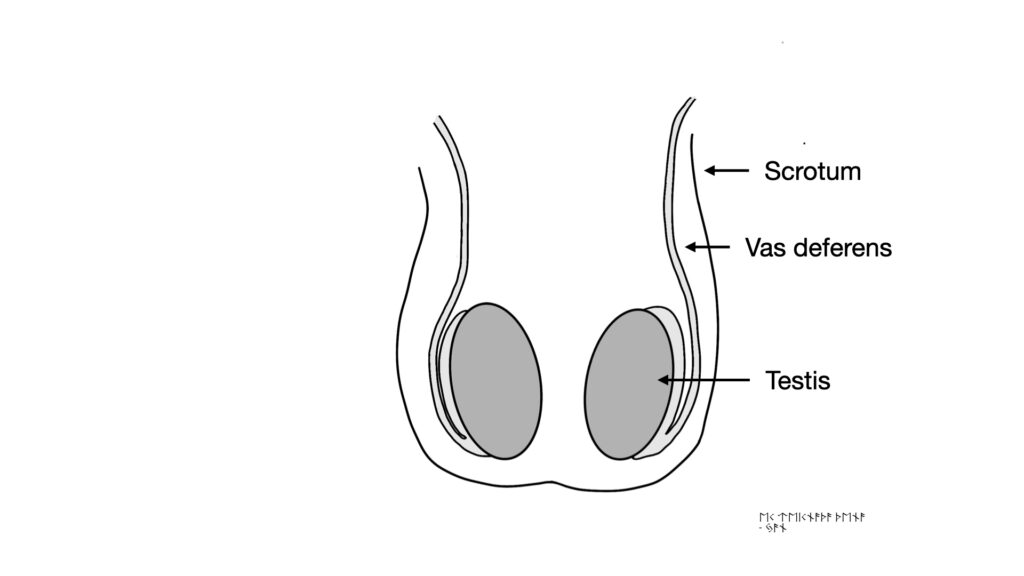
A more realistic mental representation would be to think of the large sac of the scrotum containing two smaller sacs. These smaller sacs surround the testes and spermatic cords and are composed of internal spermatic fascia and cremaster muscle.
The key concept here is that each testis is contained within its own sac and both of these sacs are contained within the scrotum. This system allows substantial control of the height of the testes. The cremaster muscles that make up the walls of the inner sacs can contract, and the dartos muscles that make up the walls outer sac can also contract, thus giving a male the ability to raise and lower the testis in response to temperature or perceived threat.
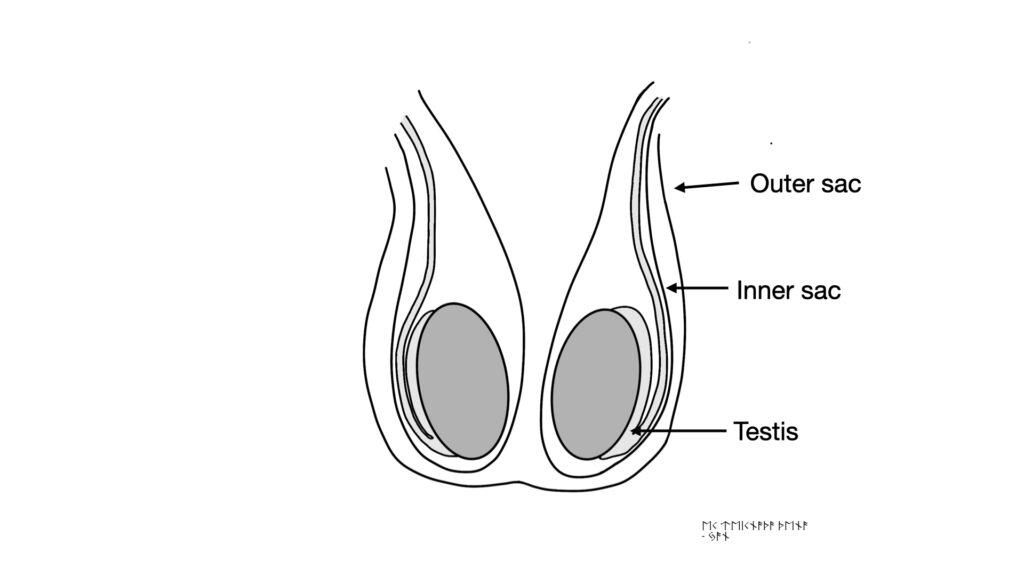
So, we can think of each testis and vas as being surrounded by a sac, and both of these sacs are contained within the larger sac of the scrotum.
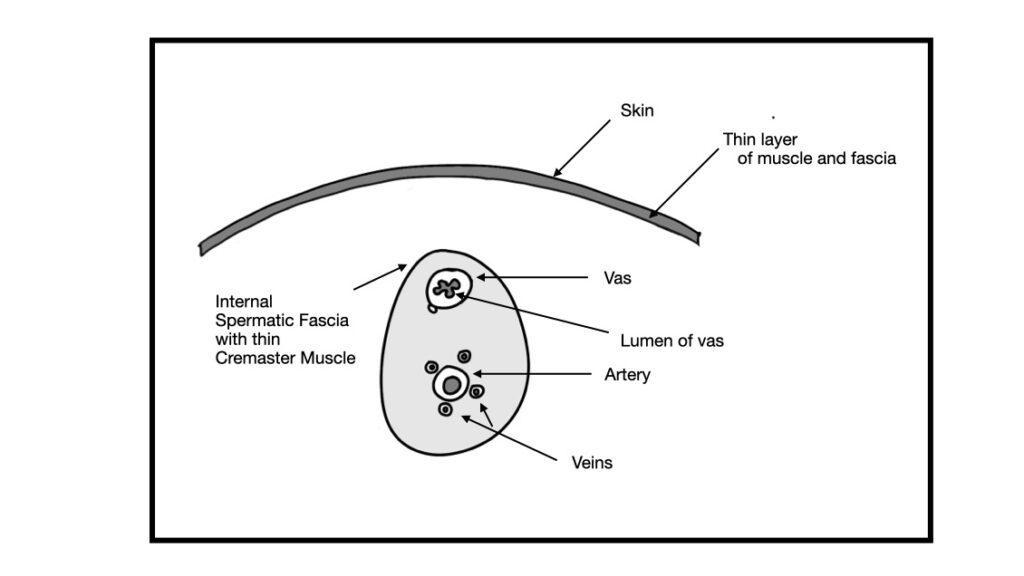
One topic that is confusing in many discussions of scrotal anatomy is the number of layers tissue that you encounter as you dissect through the skin down to the vas deferens. It has been traditional to teach that as you dissect downwards, you encounter many layers including skin, dartos muscle, dartos fascia, external spermatic fascia, internal spermatic fascia, etc. The practical reality, however, is different. During a modern no-scalpel vasectomy, we usually just perceive skin with a layer of underlying subcutaneous connective tissue, then the inner sac of internal spermatic fascia, and then the very thin layer of perivasal fascia around the vas deferens. The various other layers aren’t really perceptible during the vast majority of vasectomy cases. We’ll talk more later about the various layers and how they interact when we discuss how to isolate the vas using a ring forceps during a vasectomy.
The Testes
Continuing along with the scrotal contents, we’ll discuss the testes. The testes are where the sperm are produced. The testes are also the site of the production of testosterone. There are two testes. The singular form of testes is testis. You can also say testicle. Many patients will say “balls.” That’s nuts.
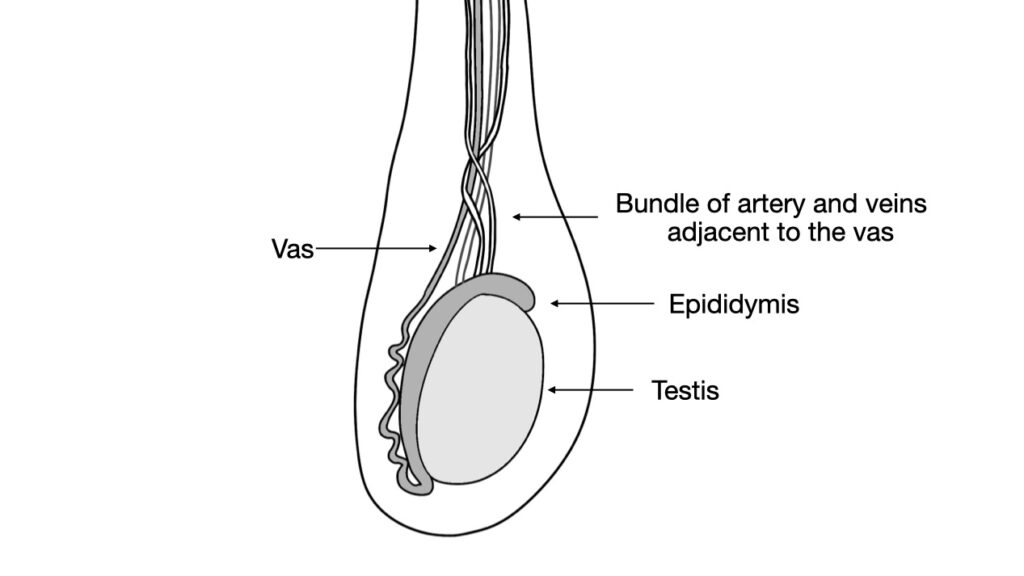
From the testis, the sperm collect in the epididymis and then travel up the vas deferens. A vasectomy is a procedure to disrupt the vas deferens, so we will keep circling around to various fine points about the vas deferens and its relationship to other parts of the male genitalia.
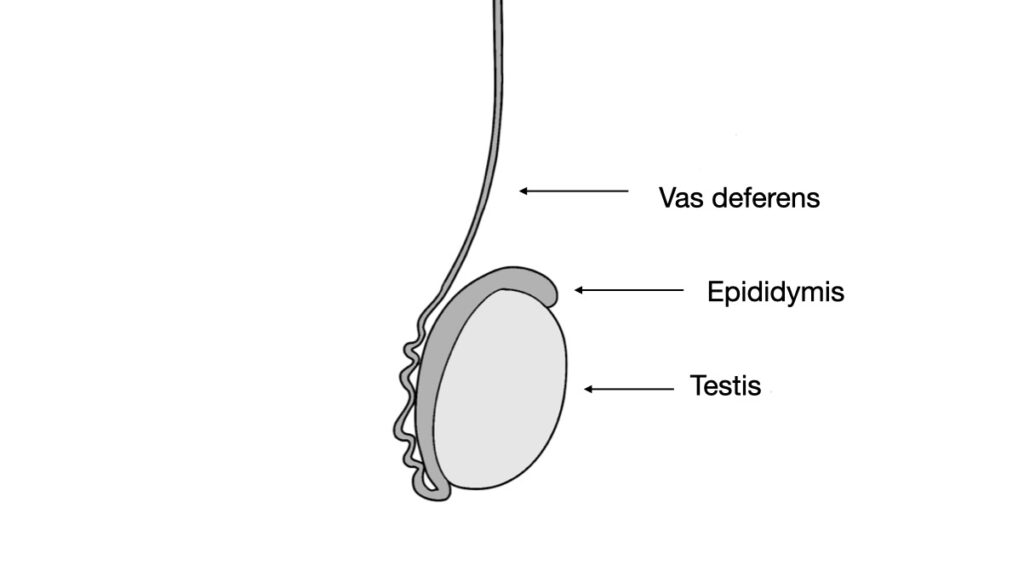
The vas deferens is the tube that carries sperm from the testis up to the prostate. The plural of vas deferens is vasa deferentia. The wall of the vas deferens is thick and muscular, and thus feels quite different by palpation from the other structures in the scrotum. The vas feels firm, while the blood vessels feel soft. The lower portion of the vas deferens – the area closest to the epididymis – is quite curvy. This section is called the convoluted vas deferens. This is important during a vasectomy since the straight section of the vas deferens is much easier to grasp, and the convoluted section of the vas is often thin-walled and more difficult to manipulate.
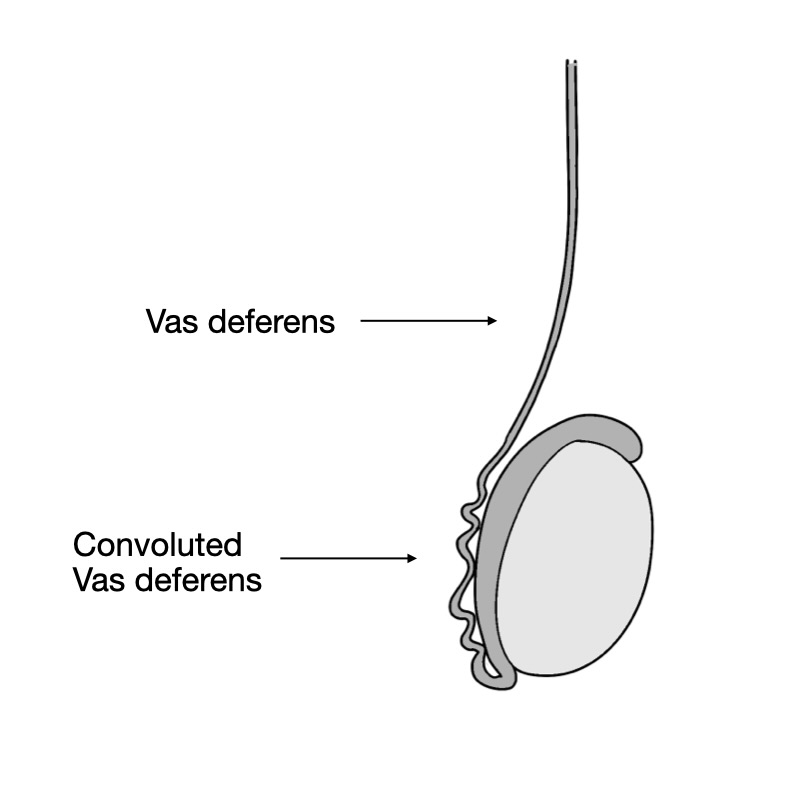
The vas deferens is surrounded by a thin layer of fascia and muscle. We know that technically this thin layer is comprised of internal spermatic fascia and the cremaster muscle. As we discussed above, however, for all practical purposes at the site of a vasectomy, the cremaster muscle fibers are so thin that we do not typically notice them.
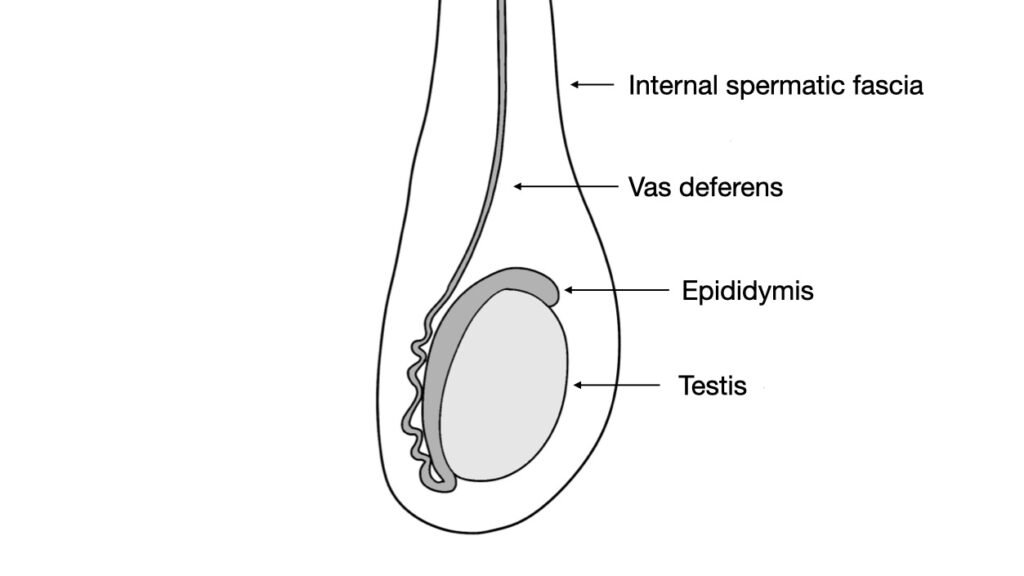
Within the spermatic cord is also a collection of blood vessels – the testicular artery and the pampiniform plexus. The pampiniform plexus is a network of small veins which serve as the vascular outflow from the testis and the epididymis. These vessels are important to mention during vasectomy counseling since these vessels carry the testosterone from the testis to the rest of the body. During a modern, minimally-invasive vasectomy , we avoid these vessels and they remain intact and fully functioning. Thus testosterone levels are not changed at all.
We now will now bring some of these concepts together and review why the various tissue layers usually feel so thin during a modern no-scalpel vasectomy, and how we keep the blood vessels safe during the procedure.
The key to the modern vasectomy is an instrument called a Li ring forceps. This was invented by a Chinese physician named Li Shunqiang.

The ring forceps serves two important purposes – it stretches the skin and fascia making them thin and easy to dissect, and also holds the vas close to the skin with the blood vessels safely below and out of the way.
We’ll talk about stretching the skin and fascia first. In the classic texts, we are taught that as we proceed downward from outside towards the vas, we will first encounter skin, dartos muscle, and external spermatic fascia. In practice, the ring forceps stretches the skin and dartos muscle and fascia so thin that they usually function as one layer from the point of the view of the vasectomist. We were also taught that below the external spermatic fascia, we encounter the internal spermatic fascia and cremaster muscle that surround the spermatic cord. With the ring forceps applied at the proper level, the cremaster muscle fibers are so thin the we typically do not perceive them. Thus, we can think of the path to the vas deferens as having two functional layers – the first a layer of skin with fascia and imperceptible muscle, and beneath that is another thin layer of fascia and imperceptible muscle. This simplified view helps us understand what we encounter during a typical vasectomy.
Below we can see the various layers before being stretched.
And below we can see the various layers stretched by the ring forceps.
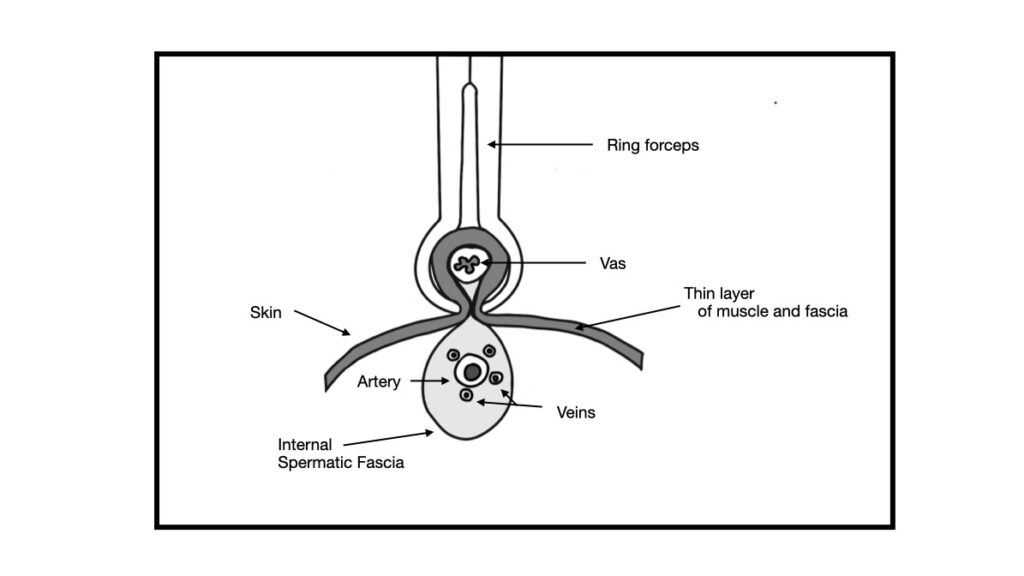
As we can see in the diagram above, the ring forceps holds the vas up against the skin and simultaneously squeezes the blood vessels within the spermatic cord safely out of the way beneath the skin. Thus, while the ring forceps is applied, we can safely access the vas deferens without damaging the underlying blood vessels.
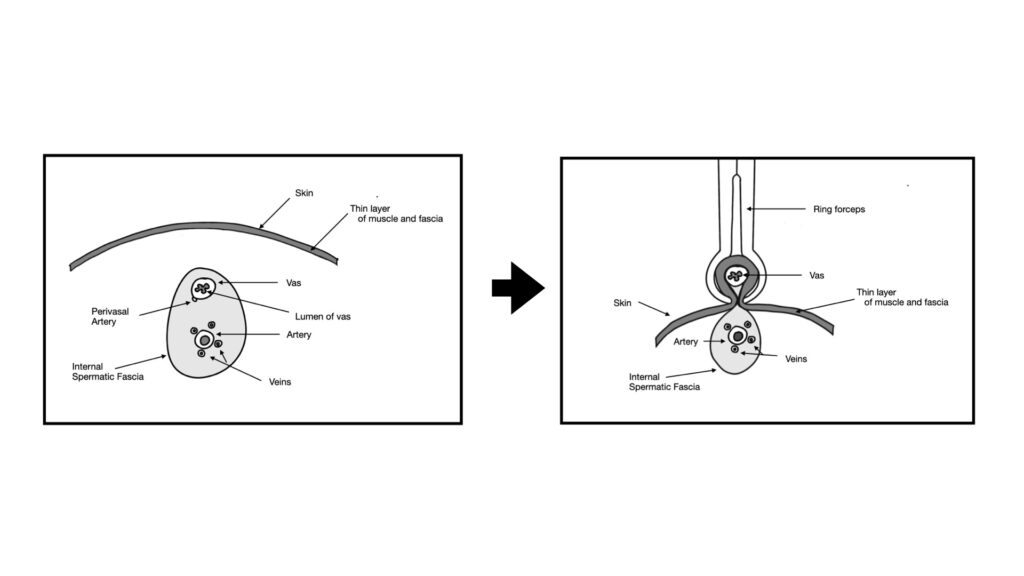
The careful application of the ring forceps is key to the safety of the modern vasectomy.
Anatomy of Semen Production
From here we’ll move on to the anatomy of semen production. By understanding exactly where the semen is produced, we can counsel patients accurately about how ejaculation works and how minimally ejaculation changes after a vasectomy. One of the key points is that sperm and semen are not synonymous. Sperm are the tiny cells that are produced in the testes. Sperm cells are the cells which can cause a pregnancy. Semen is the white liquid that comes out during an ejaculation.
Semen is produced by the seminal vesicles and the prostate, both of which are located just beneath the bladder and behind the penis.
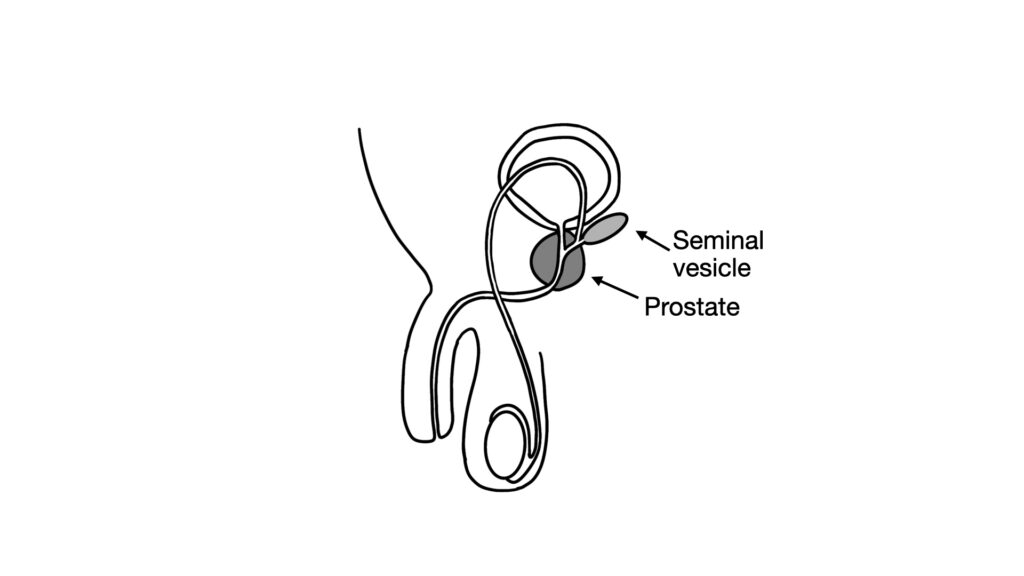
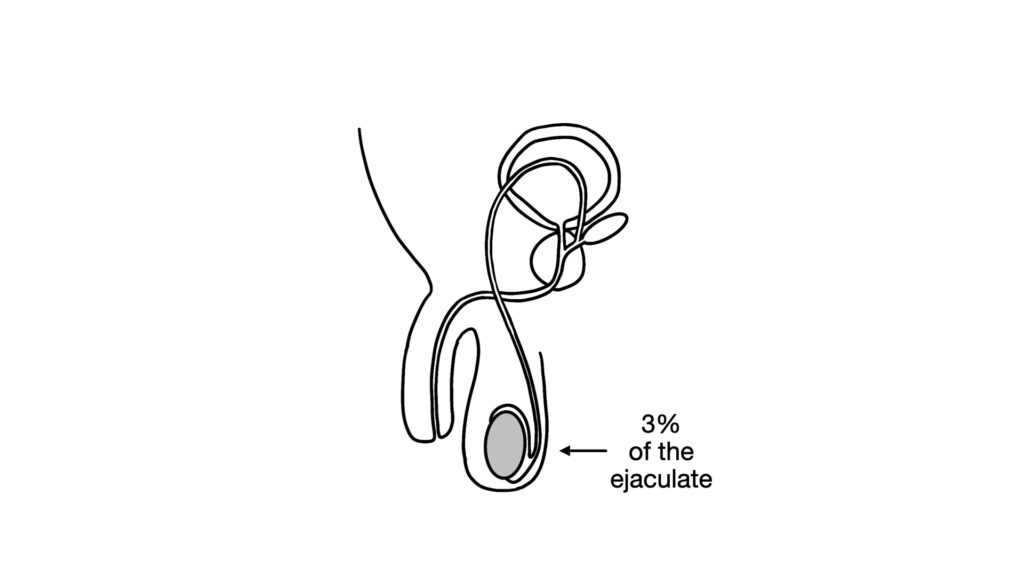
Approximately 97% of an ejaculation is the liquid made by the seminal vesicles and prostate.
Sperm is produced by the testes, and comprises only a tiny percentage of the ejaculate.
The sperm cells make up only about 3% of the volume of the ejaculate.
During an ejaculation, there are coordinated contractions of the pelvic floor muscles around the prostate, and as well as intrinsic muscles within the prostate itself. These contractions push the semen through the urethra to be expelled from the penis. During an ejaculation, a tiny sphincter closes at the base of the bladder so semen is directed into the urethra rather than into the bladder.
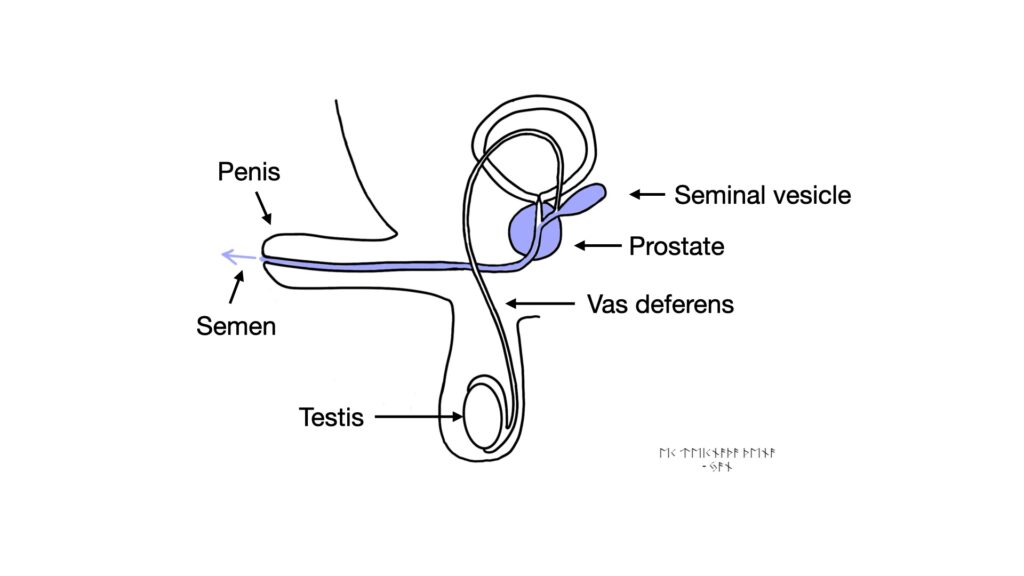
It is interesting to note that the testes do not have intrinsic muscles. Ejaculation is not caused by contractions of the testes. Contrary to popular belief, it’s not that “the balls contract and shoot out a load.” In reality, the prostate and pelvic floor muscles contract to push out the ejaculate. After a vasectomy, only the vas deferens is snipped, and the prostate and seminal vesicles are unchanged. Thus, ejaculation is essentially unchanged after a vasectomy.
Urination after Vasectomy
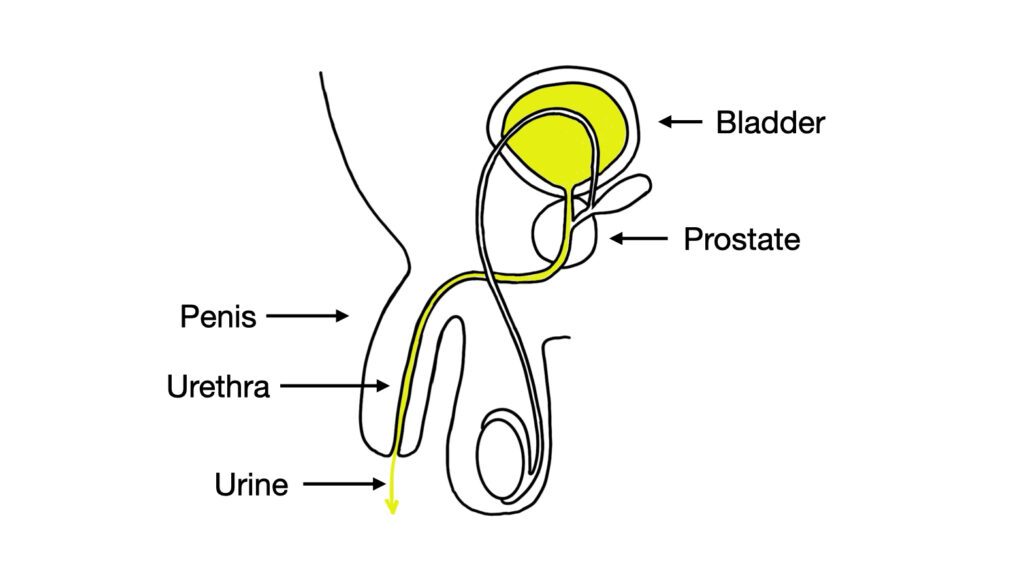
A question that comes up frequently during vasectomy counseling, is “what changes about urination after a vasectomy?”
The key concept is that the path that urine takes from the bladder to exit the body from the penis is quite distinct from the vas deferens. Making a tiny snip in the vasa won’t affect urination at all.
Summary of Vasectomy Anatomy
In short, a vasectomy works by blocking the vasa deferentia – the tubes that carry sperm. Once they’re blocked, sperm can’t reach the prostate, so they don’t get mixed into the semen and aren’t present during ejaculation.
Anatomically, very little changes after the procedure. Sex drive and erections remain the same, and testosterone levels are unaffected. Urination is also unchanged. Even the semen looks and feels almost identical – since the prostate isn’t involved in the procedure, the volume and consistency of the ejaculate stay essentially the same.